“Inlay glenoid implants are a paradigm-changer in shoulder surgery”- John Uribe, MD
In case you missed it! This interview originally appeared in Becker’s ASC Review in June 2019. Angie Stewart from Becker’s ASC Review interviewed Dr. John Uribe about his experience with the Arthrosurface joint implant systems. Check out the interview below for 7 Questions with John Uribe, MD
Joint preservation in the era of value-based care – 7 Qs with Dr. John Uribe

Inlay glenoid implants are a “paradigm-changer” in shoulder surgery, according to Miami Orthopedics & Sports Medicine Institute’s John Uribe, MD.
Dr. Uribe spoke to Becker’s ASC Review about how the approach sets his practice apart and benefits patients.
Note: Responses were lightly edited for style and length.
Q1: Can you share insights about the Arthrosurface implants you’re using and explain your patient selection criteria?
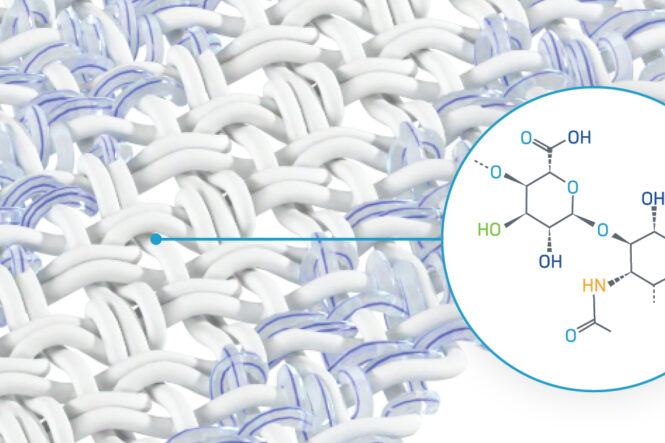
Dr. John Uribe: It’s more joint preservation that I try to specialize in, as opposed to total joint replacement. Arthrosurface is the company that does the most in terms of prosthesis to preserve the joint. I started a long time ago with partial replacements of cartilage defects in the knee, utilizing prosthesis that they made that were inlay and had the same radius [and] curvature of the bone. So, if the knee was in relatively good condition – it was just an area of cartilage that was destroyed – you could do an inlay implant.
Following those patients, I saw that the contact surface on the tibia was still preserved. That technology then was taken to the shoulder, where it started out with partial replacements of the humeral head for conditions like avascular necrosis. Then, it’s subsequently developed into a full humeral head resurfacing with an anatomic humeral head (which is not a sphere, it’s more of an oval type of shape). Then for the glenoid, as opposed to an onlay glenoid, it’s an inset or inlay glenoid. That’s basically what attracted me [to using Arthrosurface].
Q2: Why is it important to focus on joint preservation at a time when the industry is thinking about opioid reduction, value-based care, etc.?
JU: The true goal in reconstructive orthopedics has always been to restore anatomy, not really make it better. If we can preserve anatomy, or restore it to the most anatomical shape and conform it, then it is better for the patient [than] trying to do something mechanical. For example, the shoulder is a ball-and-socket joint – it’s the most unstable joint in the body – so the soft tissues play an incredible role in preserving the stability as well as the mobility of the shoulder. That’s very difficult to reproduce with the standard stemmed prosthesis and an onlay glenoid because the tension of that soft-tissue envelope is significantly impacted. And it’s just really hard to reproduce the anatomy of a shoulder. Even in the same person, that anatomy can vary – the version of the head, the angle it makes with the humerus, all that is different in people. So, if you can keep it the same for that individual, the results should be better.
Q3: How does this approach affect your practice and organization overall?
JU: You can market all you want, but the best marketing is word of mouth and patient satisfaction. When I first started doing the total shoulder with a humeral head resurfacing and inlay glenoid, I was still doing the stemmed prosthesis. It was clear after a very short period of time that the patient satisfaction, in terms of pain, function and recovery period, was much better with joint preservation with the resurfacing and the inlay glenoid.
Q4: How does this differentiate your practice when it comes to attracting patients?
JU: I had a unique subset of patients, which were the young or middle-aged bodybuilders and weightlifters that were lifting these huge weights, and over time, it crushed their humeral heads. Their humeral heads became very deformed, flattened, and [they] developed very early osteoarthritis with very limited mobility. They would probably go back to doing their activities, and the risk of loosening from the rocking-horse mechanism on the onlay glenoid was, I thought, quite high. That’s the way many total shoulders fail: the socket, or the glenoid side, gets loose.
But with an inlay, the risk of that seemed to me [to be] much less, and it subsequently has proven to be significantly less of a risk for loosening. So, these were the people I started out with, and their results were very good. They’re a cliquish kind of group, so they communicate. Pretty soon, I was getting these heavy weightlifters and bodybuilders from all over to have their shoulders replaced.
Q5: What other kinds of patients might this approach apply to?
JU: I started out [thinking], “This is perfect for the younger patients with significant osteoarthritis where there’s a lot of pain and significant loss of motion, and it’s refractory to conservative care,” because the risk of loosening and other problems with the stem prosthesis was quite high. So, when I realized after doing it with the younger individuals that I wasn’t losing much blood [and] they could go home the same day, I started using it on the older individuals, which actually turns out to be kind of the better patient. You have very little blood loss, it’s done as an outpatient, [and] the risk of, say, a fracture of the humerus or other intraoperative complications is much [lower]. So, for an elderly individual with reasonable bone stock, it’s been very good because it’s just an easier operation to get over, and functionally, they do better. Now, that’s basically my go-to procedure. The only patients I don’t use it on are individuals who’ve maybe had humeral head fractures with tuberosities that aren’t in the right position. But even with deformed glenoids – B2 glenoids or C glenoids – it’s still very effective.
Q6: You said there’s a lower risk of complications and it can be done as an outpatient. So are payers looking at this approach favorably?
JU: Yes. In fact, in the article we’ve just submitted for publication, our average blood loss was less than 100 [cubic centimeters]. In all the ones we’ve done, which is several hundred, we’ve yet to do a transfusion. And if you look at some reports of the standard total shoulders, transfusions can run anywhere between 10- and 20-some percent of cases. Plus, the only patients we’ve kept [overnight] were a few cases in which Medicare demanded that they be, or the insurance said it’s got to be inpatient. Then we discharge them the next morning, but nobody’s ever spent more than 24 hours.
You’re not cutting out any bone. You’re just scraping the humeral head and kind of reshaping it, and then putting in a cap on it. So, the risks of bone loss and fractures from your instrumentation are minimal.
Q7: Is there anything else surgeons should know about this approach?
JU: It’s a paradigm-changer to put a glenoid prosthesis inlaid as opposed to onlaid. It’s pretty significant. The key here is that you’re preserving the soft tissue envelope and the tension on that envelope. So, it should just intuitively give you greater mobility with less risk of over-tensioning, which is one of the real problems with total shoulders.
Click here to read the full article on Becker’s Spine Review.
Find a Doctor
Find a surgeon in your area who has experience with our shoulder implant systems by using our Find the Doctor tool. Don’t see anyone in your area? Contact Us and we will be happy to help!