Why Are Surgeons Choosing Our Anatomic Total Shoulder Replacement for Active Patients?
The following interview with Dr. Gregory Nicholson was featured in SmartTRAK on 4/13/20.
New research shows excellent results for anatomic TSA using a stemless humeral component with an inlay glenoid. Dr. Gregory Nicholson gives the breakdown on the research, indications, market acceptance and limitations.
In the market for total shoulder arthroplasty (TSA), younger, active patients with degenerative conditions of the glenohumeral joint are a unique and more complicated population for surgeons to treat with TSA. Challenges in treating this cohort include higher functional demands that can lead to implant wear and failure. However, a recent study suggests a new implant design might be a good option for these types of patients, potentially filling a treatment gap and expanding the market for TSA. [cont.]
The study, recently published in the Journal of Elbow & Shoulder Surgery, reported results of TSA in younger, active patients treated for osteoarthritis with a stemless ovoid humeral head and an inlay glenoid. The study concluded anatomic total shoulder replacement with this implant design, Arthrosurface’s OVO with Inlay Glenoid Shoulder, resulted in improved clinical outcomes with no reoperations or radiographic loosening in 27 shoulders with a minimum two-year follow-up. And, at an average 3.7 months, the return to work rate was 92.6%.
One of the study investigators, Gregory P. Nicholson, MD, Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, sat down with SmartTRAK’s Lisa Mahan to discuss the study results and how this implant design affects the treatment of shoulder osteoarthritis in younger patients.
SmartTRAK: Could you give us a summary of the study, your involvement in the study, and then highlight some of the key findings?
Dr. Gregory Nicholson: This design evolved out of what we used to do for younger patients who needed a shoulder replacement because of arthritis. We identified polyethylene as the weak link. We tried other things such as hemiarthroplasty alone, reaming the native socket to a little bit better shape – ream and run, to putting in an interpositional implant or an achilles tendon allograft or other type of tissue in the shoulder. But, the best combination for pain relief and function restoration was actually a well-done total shoulder. Even so, for those people who are younger, in the workforce and who also have demanding occupational and/or recreational activities, it would give us some pause about putting a little plastic socket in that we knew was going to wear, change shape or potentially loosen with that kind of activity.
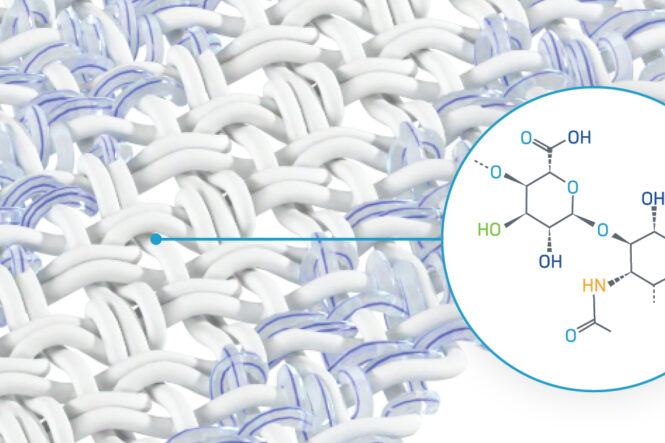
So the Company [Arthrosurface] came up with an idea to address the issues associated with the conventional implant design of putting an inlay at the face of the glenoid in the center of rotation, kind of like a tile in the middle of your floor that’s flush, as opposed to the onlay glenoid. The Company also realized the shape of the humeral head was actually aspherical – longer lateral to medial than anterior to posterior and designed a more truly anatomic humeral component.
In these high-risk patients, I was skeptical when I started and I remain wary, but as time went on our practice took on more and more “higher risk” patients – guys in the workforce, guys who lift weights. Obviously, we need long term follow-up. But as we follow these patients, they’ve had a remarkable restoration of motion and increased activity level compared to a standard shoulder replacement. Their pain relief has been excellent. It’s not for everybody, but then everybody says, well why don’t you use it on everybody if it’s that good? I don’t have an answer for that one right now.
We decided that we were going to take these high-risk patients, 95% of them are men who are in the workforce, or into recreational activities that are troublesome, and we were going to use this implant and treat the patients as we did with all total shoulders. After surgery, they would get back to work and they would do stuff you normally wouldn’t want them to do. So we said, we’ve got to look at these. A friend of mine, Dr. Tony Miniaci at the Cleveland Clinic, who was kind of behind the implant, had a parallel series going on at the same time. Our two papers have come out within months of one another, mine and his, and it’s really shocking the similarities of age, gender, activity, range of motion and results. In this really active population, at this short term and I would call it a mid-term even, we’ve had a very, very good return to work level. Very, very good return to recreation level, range of motion satisfaction and no revision issues at this point in time.
Did this particular shoulder design open up treatment for that higher risk population? You talked about the workforce, the men that were lifting weights or participating in intense activities, did this give them an option that wasn’t there before? Or maybe there wasn’t an optimal option?
GN: There wasn’t an optimal option and we would compromise. If you look at studies on standard anatomic total shoulders in patients under the age of 50 or around 50, they work great. The numbers are great, the patients love it, but they have an early failure rate. I mean, anywhere from 18 to 35 to 50% revision within five to eight years.
But with this implant design, you can get theses younger active patients back to a higher level of work or what they did before, be it a cop or a fireman or a truck driver, a painter, or just someone who wants to continue to lift weights, play golf, that kind of stuff. So I don’t think it’s the absolute solution, it’s certainly a good one, but I would say now we have another tool in our toolbox as a shoulder surgeon to offer these particular patients an implant that performs well, gives them excellent range of motion, excellent pain relief and hopefully avoids some of the failures that we saw.
The other thing with this inlay glenoid you get almost a symbiotic relationship with the face of the glenoid. The face of the bony glenoid protects the inlay from wear and liftoff and the plastic inlay protects the bony glenoid from wearing medially. I can’t quantitate it right now, but as time goes on that’s what we’re seeing. Also, it is a bone preserving operation, both on the glenoid side because there’s no pegs and no keels and on the humerus side with very minimal bone being removed. Because things are going to happen and people are going to need to have a revision for one reason or another, you’ve got more playing field left, if you will, down the road. You’ve got more bone stock down the road if you have to do something. So there’s a lot of advantages to it.
This study was focused on younger, active patients. However, do you feel this design will carry over into treating other patients with other indications such as rheumatoid arthritis?
GN: Rheumatoid arthritis is an inflammatory arthritis and sometimes the bone isn’t very good so you‚Äôve got to be very careful or the rotator cuff might not be very good. And for somebody in their 60s or 70s, or for those with a really small anatomy, that type of thing or for a fracture, you may need a stemmed humeral implant.
There is another total shoulder on the market that also has an inset glenoid paired with either a short or standard length humeral component, the InSet Total Shoulder from Shoulder Innovations. It also has a study published in the Journal of Elbow & Shoulder Surgery showing statistically significant improvements in outcomes and functional results with no revisions at an avg 8.7 years follow-up. Do you have any experience with this implant and how do you feel it compares to the OVO with Inlay Glenoid Shoulder?
GN: The glenoid is a little bit more of an inset compared the OVO’s inlay, meaning it covers the whole surface of the glenoid shape. It is inset into the subchondral bone, so in my mind there is more machining of entire surface. Also, the humeral head is not the aspherical shape of the implant that was in my study, the OVO Motion. I can’t really give you a comparison between the systems. I have not used this implant [InSet Total Shoulder] in a patient.
In your practice, what’s the percentage of how often you use this type of implant versus doing a reverse shoulder?
GN: So worldwide and in the United States now, about 60% to 65% of all shoulder replacements are reverse shoulder replacements because the indications for a reverse are much broader than an anatomic total shoulder. An anatomic total shoulder is indicated for those people with shoulder arthritis with a good intact functioning rotator cuff that’s rehabilitatable and have adequate glenoid bone stock.
With a reverse, it’s failed rotator cuff repairs, rotator cuff deficient arthritis, elderly people over 75 with arthritis because they’ll do very well and won’t have to do as much rehab. There’s just a broader indication. So when I look at my anatomic total shoulder patients out of that segment, I think almost 80%, 90% of them would be appropriate for this type of implant.
Have you had the opportunity to talk to other surgeons about their experience with this implant design? What was their feedback?
GN: Yes and it’s like any new implant. There’s a learning curve to any new implant or any when you change over, but when people have used it and they’ve seen the results, they are quite intrigued, they’re quite pleased and universally the response has been very, very good.
Do you have any visibility to how this design has been in terms of physician adoption? What’s driven it and are there are any limiters?
GN: I think exposure to the socket. The glenoid is always difficult and a modification on the humeral side was done about three years ago, which allowed a little more bone removal, better visualization to the socket, easier implantation. That has really made this more reproducible, less strenuous for somebody who hasn’t seen it, because you need a certain exposure, you need to be able to get to where you need to get. You’ve got to be an active shoulder surgeon who does a fair amount.
Also, it’s a little bit of a smaller company so it doesn’t offer a hip replacement, things that might be bundled for a hospital system. But our charge is to give our patients the best result we can give them. What do patients want? They want predictability and they want durability and they want a return to the things they want to do and I think this implant checks all those boxes.
Learn More!
To learn more about the Arthrosurface shoulder implant systems visit our site.
Feel free to contact us with any questions or email us at hope@arthrosurface.com!